
When you are a member of Medical Protection, you benefit from more than 125 years of experience defending doctors and other healthcare professionals. That isn’t just a number. It’s more than 12 decades of specialist expertise that we use to protect members long into the future.
As a global organisation we are committed to getting as close to our members as possible, providing a tailored service that supports you in dealing with issues of local relevance and urgency. Our support for members is more accessible than ever before and our Ireland-based team of experts includes doctors with medicolegal knowledge and clinical experience of GP work.
At the heart of our business is a philosophy of supporting safe practice and helping our members avert problems from happening in the first place. You can see this commitment through the learning resources we offer, including a host of professional development courses and ongoing learning and development opportunities.”
Rob Hendry
Medical Director
Medical Protection
Introduction
Diane Baylis, Clinical Risk Educator and Dr James Thorpe, Senior Medical Educator and Medicolegal Consultant, look at the reasons behind medicolegal cases reported to us at Medical Protection.
We’ve developed this collection of case studies, statistics and analysis from our extensive library to give you a view of the current claims landscape for general practice.
The accompanying learning points also help you avoid the problems others have faced.
Read this resource to:
- Understand common themes from general practice cases in Ireland in which we have supported members.
- Receive tailored advice and key recommendations to help you reduce risks in the future.
Background
Medical Protection’s expert team provide support to our GP members for medicolegal matters arising from professional practice. This can include complaints to the Medical Council, advice and expert representation for coroner’s inquests and general advice on the many legal issues that can arise in medical practice.
Claims for compensation in general practice can lead to large financial settlements. The value of the settled claim will often include compensation for care and loss of earnings, if applicable, in addition to an award for the damage that resulted from a breach of duty. The value of each claim varies enormously with our highest GP total case payment (claimant damages, costs and legal costs), being in excess of €8m.
The decision to take legal action is influenced not only by the original injury, but also by the patient’s perception of how information was provided and whether, or how, an explanation and an apology were given.
We understand you work in complex and pressured environments. We know from member feedback that experiencing a medicolegal case can be concerning and a source of stress. At Medical Protection we want to share our knowledge, experience and expertise with you in order to support you in your everyday clinical practice.
Purpose
Highlight common pitfalls and themes to support GP members, to learn from these cases and mitigate risk. Based on this collective experience we will provide tailored advice and key recommendations to help you reduce future medicolegal risks.
Analysis
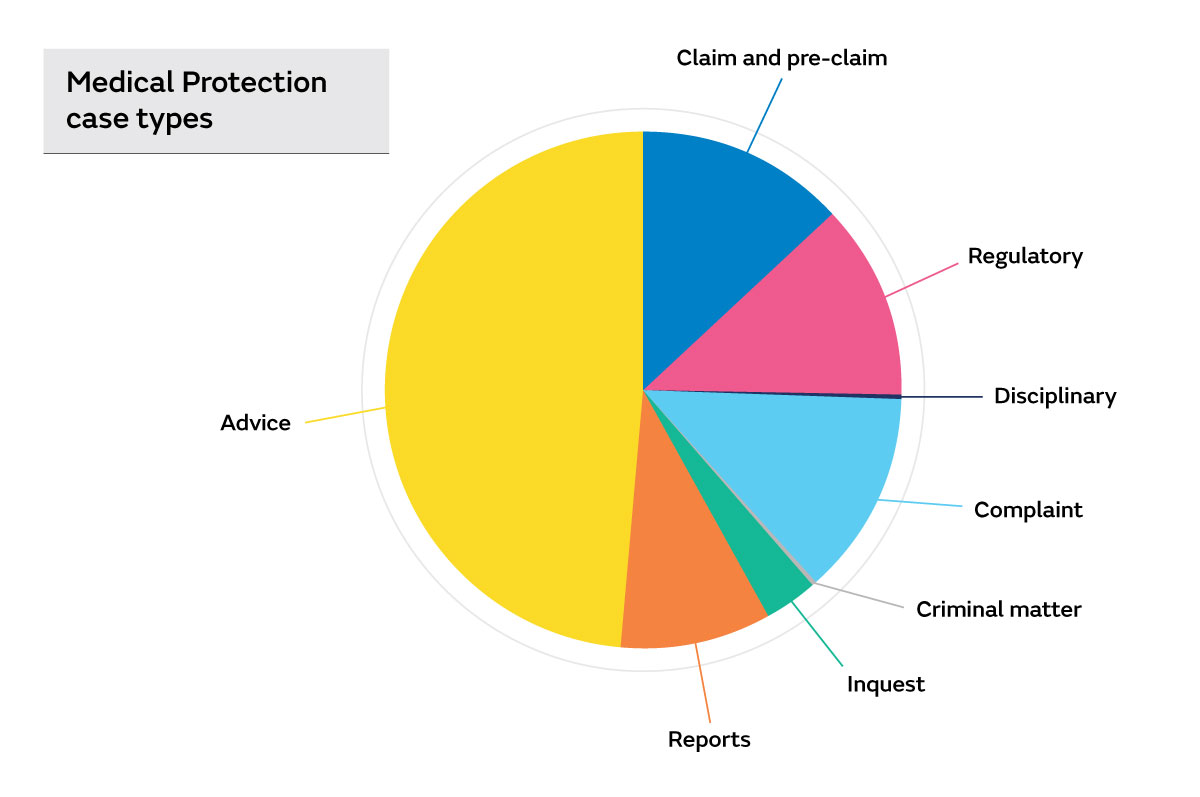
Analysis of over 2,000 Medical Protection cases involving GP members over a 3-year period (2017-2020) was undertaken. Almost half of these cases related to requests for advice on a wide range of legal and professional issues, for example:
- Disclosure of records to solicitors/ An Garda Síochána
- Release of deceased patient records
- Indemnity arrangements
- Testamentary capacity
- Safeguarding responsibilities.
Around 14 percent of cases were opened to provide expert assistance to members responding to Medical Council complaints, while a similar number were opened to provide support to members who had been notified of a complaint directly to the practice.
We assisted our members to draft responses and disclose medical reports requested for a variety of purposes, including:
- Hospital investigations following an adverse incident
- Requests by solicitors and insurance companies
We also assisted GP members when approached by the coroner in relation to an inquest. This included arranging appropriate independent legal representation.
Between 2017 and 2020, we assisted with over 300 claims (demands for monetary compensation including allegations of negligence) or pre-claims (intimations from a claimant of a possible claim for compensation).
We have analysed all claims including those defended, settled or discontinued. Sharing insights of why patients decide to take legal action and identifying vulnerabilities which lead to claims being settled can help our members to mitigate risks.
Common themes identified in claims
One quarter of the claims and pre-claims involved a delay in the diagnosis of cancer. The remaining three quarters of claims and pre-claims involved a wide range of clinical conditions. Of these cases, over 50% involved allegations of a delayed diagnosis or a failure to refer a patient to secondary care appropriately. A wide range of clinical conditions were the focus of allegations, but a number of claims related to the following pathologies:
- Delayed or missed diagnosis of Cauda Equina Syndrome
Several claims arose from alleged failure to appropriately investigate back pain or refer patients subsequently diagnosed with Cauda Equina Syndrome for hospital assessment. Claimants cited a range of long-term neurological sequelae ranging from persistent perineal numbness to incontinence and limited mobility.
- Delayed or missed diagnosis of appendicitis
Some claims related to alleged delays in the referral of patients subsequently diagnosed with appendicitis, often requiring more extensive surgical treatment or complications as a result of an appendix abscess or perforated appendix.
- Delayed or missed diagnosis of peripheral vascular disease
Alleged delays in the diagnosis of, or referral for investigation of, peripheral vascular disease were cited by several claimants requiring major lower limb amputation.
- Delayed or missed diagnosis of cardiac chest pain
Alleged missed or delayed referral of cardiovascular disorders including myocardial infarction led to some claims.
Key learning points:
- Thorough documentation of consultation including both positive and negative examination findings increases the chance of successfully defending claims
- Failure to refer or take further action in the presence of ‘red flag’ symptoms was a common allegation in relation to Cauda Equina Syndrome
- In defending a claim of clinical negligence you must be prepared to explain and justify your management decisions
- Evidence of appropriate ‘safety netting’ advice is important when defending allegations of negligence.
Case example
A 56-year-old female patient presented to practice with significant back pain and was prescribed opiate analgesia for a ‘slipped disc’. The GP made brief records and did not record whether ‘red flag’ symptoms (for example leg pain and change in bowel/ bladder function) were present or absent. In addition, no clinical examination findings were documented.
The patient was seen by another GP 72 hours later, with ongoing back pain and perineal numbness. She was admitted to hospital and required urgent surgery after being diagnosed with Cauda Equina Syndrome. She was subsequently left with long-term neurological sequelae including a degree of incontinence.
The patient later submitted a claim for negligence against the GP alleging that she should have been referred to hospital at the time of the initial consultation with back pain. Evidence was obtained from a GP expert witness who was critical of the record keeping and lack of documented examination. The case was ultimately settled out of court for a large sum.
Medication and prescribing errors
More than 15% of claims involved alleged medication or prescribing errors. Issues relating to medication errors have the potential to result in serious harm. Common issues identified were:
- Lack of monitoring of high-risk medication including lithium and warfarin
- Lack of monitoring of long-term medication (e.g. renal function in antihypertensives) and failure to maintain monitoring
- Lack of clarity over who is monitoring, in cases of shared care between primary and secondary care
- Prescribing incorrect doses of medication
- Prescribing the wrong medication with a similar name to the intended drug
- Inappropriate repeat prescribing
- Failure to review the need for ongoing medication
- Inappropriate prescribing in pregnancy.
Case example 1
A 40-year-old female patient received the incorrect, suboptimal dose of her medication following discharge from hospital. The practice secretary had inputted the incorrect dose when updating the patient's medication list from the hospital discharge letter. The error was not identified by the GP who signed the prescription and the patient continued to take the medication for one month before the error was discovered.
Key learning points:
- Non-clinical staff should not be allowed to input or update medication on the practice computer system and records
- GPs must check the prescription prior to signing. Check the dose, frequency and route.
Case example 2
A 57-year-old male patient registered with a new GP practice. At the time of registration his regular medication, including lithium, was added to his repeat prescription. Over a two-year period, the patient repeatedly received his prescription from the practice, but blood lithium levels were never monitored. This ultimately resulted in the patient being admitted to hospital with lithium toxicity.
Key learning points:
- Ensure that you have robust practice systems in place for the monitoring of patients taking high risk medication
- Undertake annual reviews for patients on repeat prescriptions
Sodium valproate (Epilim)
There were several cases with allegations relating to failure to alert the patient to the potential risks of the use of sodium valproate (Epilim) during pregnancy, some resulting in the child suffering with severe learning difficulties /Foetal Valproate Syndrome.
Sodium valproate is associated with a significant risk of birth defects and developmental disorders in children born to women who take valproate during pregnancy. In 2018, the European Medicines Agency recommended new restrictions on the use of sodium valproate and it must no longer be used in women or girls of childbearing potential unless the terms of the Valproate Pregnancy Prevention Programme are followed1.
Procedures and minor surgery
Around 10% of claims involved allegations arising from procedures or minor surgery performed within the practice setting. The following were the most common leading to litigation:
- Mirena coil insertion - A number of claims arose due to migrated devices resulting in patients requiring laparoscopy for removal. Other complications arising during insertion, such as perforation of the uterus or alleged inadequate follow-up, were also observed
- Vasectomy - Complications arising from vasectomy, including haematoma and failure of the procedure, resulted in litigation
- Cryotherapy - Multiple claims were observed following cryotherapy, with claimants citing alleged excessive scarring, hypopigmentation or blistering as a result of treatment
- Venesection and IM injection - Alleged complications from venesection or IM injection including nerve damage, abscess formation or post-procedure collapse, resulted in requests for compensation
Key learning points:
Ensure that the patient is fully informed of:
- The aim of the procedure, what it entails, and what you would consider to be a successful outcome
- The risks and benefits of the procedure
- Ensure that you keep up to date with current best practice on performing the procedure.
Delayed diagnosis of cancer cases
One quarter of all claims involved an alleged delay to the diagnosis or treatment of cancer.
Of those cases, nearly half were regarding female cancers; breast, cervical and endometrial cancer, with breast cancer being the most frequent cancer involved in the claims reviewed.
Outside of the female cancers, prostate cancer was the most common cancer mentioned in claims, with lung cancer, pancreatic cancer and malignant melanoma being the next most common.
The age of patients varied from 22 to 74 years, with 66% being aged 50 years and under. Nearly three quarters of the cases involved female patients.
Common systems issues and contributory factors identified included:
- Inadequate or poor record keeping
- Referral delayed and not followed up
- Referral not sent as urgent or an urgent referral not followed up
- Missed and lost referrals
- Misinterpretation of test results or a failure to act on abnormal test results
- Failure to refer to a specialist at an earlier point in time
- Failure to follow up and investigate.
Case example 1
A 55-year-old female patient attended her GP with shoulder pain. The GP referred the patient for lumbar and thoracic X-rays. The X-rays reported abnormalities with reference to metastases, but the GP missed the abnormal report.
After repeated attendances over a six-month period, a diagnosis of breast cancer was only made when the patient reported distortion of the right breast and inverted nipple and was referred urgently to the breast clinic. Sadly, the patient was diagnosed with metastatic breast cancer.
There was a delay in diagnosis leading to a reduced life expectancy. Therefore, the case was settled for a large sum.
Issues that contributed to the delay in diagnosis included:
- Poor record keeping with several attendances where no clinical notes were recorded
- The GP missed the abnormal X-ray report.
Key learning points:
- Ensure robust and reliable practice systems for the review, action and follow up of all test results
- Maintain complete and contemporaneous record keeping of all patient interactions and consultations.
Case example 2
A 52-year-old male patient with a family history of prostate cancer was advised by their GP to have a PSA (prostate-specific antigen) test. The result showed an elevated PSA level but the patient was not informed. He subsequently attended the GP on several further occasions with unrelated issues. The GP did not discuss the raised PSA test results and the patient did not request the test results.
Four years later, the patient attended complaining of frequency of micturition and his PSA was repeated and again found to be elevated. Rectal examination revealed an enlarged prostate gland and he was referred immediately to the rapid assess prostate clinic. Unfortunately, he was diagnosed with prostate cancer and required a radical prostatectomy.
Issues that contributed to the delay in diagnosis included:
- Abnormal test results were not relayed to the patient
- The GP did not record a digital rectal examination at the time of the first raised PSA results
- The patient should have been referred, as well as being asked to attend for a review and repeat PSA. The GP stated that he intended to refer the patient to the rapid access Urology clinic. However, he could not recall whether he made the referral
- The records were generally poor and lacking in detail.
Key learning points:
- Ensure robust practice systems for the review and follow-up of test results
- Ensure robust practice systems to identify missed referrals
- Maintain complete and contemporaneous record keeping of all patient consultations and referrals
- If GPs routinely check the last few consultations and results prior to seeing the patient, any abnormal test results should be picked up and this situation should be avoided.
Record keeping issues
Good medical records are a vital component of providing high quality, safe patient care and they are often viewed as a reflection of the standard of care that was provided. The quality of medical record keeping in general practice is highly variable. Poor record keeping can have adverse consequences such as a delayed diagnosis leading to a complaint, claim or referral to the Medical Council.
One in five cases identify record keeping issues.
Common issues identified are:
- Illegible handwriting
- Inadequate record or no record of the consultation
- Poor documentation of consent or no documentation about the risks of treatment
- Failure to record significant aspects of relevant history and examination findings
- No documentation on decision making or plan for review
- No documentation of safety netting advice.
Key learning points:
Adopt a structured approach to record keeping and remember the minimum standards:
- Context
- Consent
- History and assessment – including examinations and observations
- Options based on diagnosis
- Safety netting
- Follow up.
This will help to ensure that your documentation is maintained at a high standard and is as accurate as possible. It will also help to demonstrate that satisfactory assessment and decision making has taken place, ensuring patient safety and, importantly, helping to protect you against future claims and complaints.
Issues regarding consent
A significant proportion of the clinical negligence claims and complaints included allegations of failure to obtain valid consent, specifically:
- Lack of discussion and documentation of risks and benefits of treatment or procedure
- Failure to document discussion regarding alternative treatments
- The consent form used was inadequate, often in that it did not list the specific risks or side effects of the procedure or treatment.
For consent to be valid, the patient must have the capacity to make the decision in hand and sufficient knowledge and information on which to base a decision. The provision of information is key to obtaining valid consent. Discussion of all the issues surrounding a proposed investigation or treatment is an integral part of the patient’s clinical care. These discussions may take place over several consultations, all forming part of the consent process.
The quality and clarity of the information given is the paramount consideration. The information provided should include:
- Aim of the procedure or treatment and what it entails
- Risks and benefits of the treatment or procedure
- Alternatives to treatment – which could include doing nothing, if appropriate. (This is a dominant issue currently in some of our high value claims)
- Major risks and minor but important risks.
The above should be documented as well as any questions the patient has asked, answers given and the patient's apparent understanding.
Patients should, wherever possible, be given time to consider their options and an opportunity to ask any questions before deciding to proceed with a proposed treatment.
Patient complaints - common themes
In our experience patients often direct a complaint to the Medical Council, as many practices do not have an in-house complaints procedure which may divert from the Medical Council and the legal route. When we analysed the patient complaints reported to Medical Protection, there were some similar themes to the claims, but also some new themes:
- Patient complaint regarding inadvertent breach of confidentiality
- Poor manner and attitude – some complainants alleging poor behaviour of the staff in the practice
- Alleged impropriety during the consultation.
Regulatory cases – common themes
In regulatory and disciplinary cases, complaints can arise from patients as well as senior and junior colleagues and can be related to clinical and non-clinical issues.
Themes of issues reported to the regulator are similar to those of claims, but also include the following:
- Inappropriate personal behaviour or misconduct
- Poor communication with colleagues or patients
- Alleged inappropriate prescribing of medication
- Member health issues
- Alleged incorrect billing
- Alleged breach of confidentiality
- Various issues relating to the removal of patients from lists.
Top tips to minimise risk
Please note this is not an exhaustive list of recommendations but key learning points from our analysis:
Ensure your practice protocols are regularly updated and in line with current best practice which would be supported by your peers.
Listen to what your patient would consider to be a successful outcome following any treatment. Understand their concerns and expectations.
Discuss the possible benefits and risks of all potential treatment options. Consider what is most important to that individual taking into account their current employment.
Explain what the procedure or treatment will involve, and any follow up or blood monitoring that is required.
Ensure reliable systems are in place to follow up test results.
Double-check that the information has been understood and decisions are correctly informed.
It is important to remember that what can be classed as an intimate examination may depend on the individual patient.
Clearly document all the steps to provide evidence of a detailed interactive discussion; this is vital for legal purposes.
Remember that accurate and clear documentation, which often may need to be relied upon years after the event, are the cornerstone of any medicolegal defence.
When things go wrong, most patients just want two things: an explanation and an apology.
Ensure you are fully indemnified to carry out the relevant procedure in the Republic of Ireland.
Earn CPD on this report
Supporting continual professional development
With over 125 years’ experience, we know that the most effective way to protect our members is to help them avoid problems before they happen. Through our dedicated online learning hub, PRISM, we provide access to a wealth of learning resources to support ongoing professional development to help mitigate risk. .
Designed to fit around a busy schedule, many of our learning options are available on-demand and are a simple and convenient way to earn CPD. Our members can choose from online courses, webinars, workshops, masterclasses and podcasts. We cover a wide range of topics and all are designed and delivered by medicolegal specialists and leading medical experts.
If you’re a member you can find out more and activate your PRISM account at prism.medicalprotection.org
If you’re not a member but would like to find out more about the benefits of joining Medical Protection, visit medicalprotection.org/ireland/membership
Additional sources of information and opportunities for professional development
Medical Protection Workshops, such as Mastering Shared Decision Making
Achieving Safer and Reliable Practice
Medical records for GPs
Medical Protection’s online learning hub, PRISM
Online learning modules, including Communicating risk, Preventing complaints and communication after on adverse event
MPS case reports
MPS factsheets
References
- HSE guidance, Valproate (Epilim)
https://www.hse.ie/valproate
About the authors
Diane Baylis is a Clinical Risk Educator in the Risk Prevention department of Medical Protection. She develops and delivers education for our members in order to improve the quality and safety of patient care and reduce avoidable harm to patients. She has worked extensively with members in Ireland and presented at many of our conferences and events. She has an MSc in Risk Management in Health Care.
Dr James Thorpe is a Senior Medical Educator in Medical Protection’s Risk Prevention team. James joined the organisation in 2014 as a Medicolegal Consultant assisting members in Ireland with medicolegal issues arising from their professional practice. James trained in general and vascular surgery, is a fellow of the Royal College of Surgeons of Edinburgh and has an LLM in Medical Ethics and Law.